ArtÃculo Original
Incidence rate of long-term infective endocarditis after transcatheter aortic valve implantation
A MatÃas RodrÃguez-Granillo, Camila Correa-Sadouet, Hernán Pavlovsky, Juan D Orellana, LucÃa Fontana, Carlos Fernández- Pereira, Juan Mieres, Norberto G Allende, Valeria Curotto, Alfredo E RodrÃguez
Revista Argentina de Cardioangiología Intervencionista 2021;(3): 0128-0131 | Doi: 10.30567/RACI/20213/0128-0131
Background. Reports on the incidence rate of infective endocarditis (IE) after transcatheter aortic valve implantation (TAVI) are scarce and limited to case reports and international registries, without information coming from our own country. The objective of this study was to know the long-term incidence rate of this entity, its microbiological profile, and the clinical results in an effort to assess strategies that may prevent and treat this disease in our region.
Methods and Results. We retrospectively analyzed the TAVI registry of all consecutive patients who received the device from 3 centers from the Centro de Estudios en Cardiología Intervencionista, Patients were included in the study from 2009 through March 2020 (n = 122). We used the Modified Duke criteria to adjudicate the occurrence of prosthetic valve infective endocarditis (PVIE). We categorizedPVIE based on the time elapsed since the early procedure into early PVIE (from 0 to 60 days), intermediate PVIE (from 60 to 360 days), and late PVIE (after 1 year). Also, we assessed the baseline clinical data, as well as the follow-up results and microorganisms found on the cultures. The SPSS v. 17.1 statistical software package was used for statistical analysis. The mean age was 82.5 +/- 7.3 years, and 52.7% of the study sample were male patients. A total of 54.9% of the TAVIs performed used self-expandable valves. Femoral access was used in 83.7% of the patients, and 5.4% were already carriers of a definitive pacemaker when the procedure was performed. A total of 18.4% of the patients needed pacemaker implantation after the procedure. The average hospitalization time was 6.4 +/- 5.8 days. The complete follow-up time was 1064 +/- 488 days and the incidence rate of PVIE was 2.4%. Staphylococcus epidermidis was isolated in 2 cases and Enterococcus faecalis in 1. Conventional surgical aortic valve replacement was achieved in 1 patient with PVIE, and 1 patient was successfully treated with antibiotics. The overall mortality rate due to PVIE was 33%.
Conclusion. The incidence rate of PVIE in our population was low, which issimilar to the incidence rate reported in other regions. The prophylactic strategy and treatment used must be directed to the common microorganisms reported in the medical literature available.
Palabras clave: prosthetic valve endocarditis, TAVR, TAVI, infective endocarditis.
Antecedentes. Los reportes acerca de la incidencia de endocarditis infecciosa (EI) luego del implante percutáneo (TAVI) es baja, estando limitada a reportes de casos y registros internacionales, sin existir datos de nuestro país. El objetivo de este estudio fue el de conocer la incidencia a largo plazo de esta patología, el perfil microbiológico y los resultados clínicos, a fin de mejorar estrategias de profilaxis y tratamiento en nuestro medio.
Métodos y resultados. Se analizó de forma retrospectiva el registro de todos los pacientes a los que se les implantó una TAVI por estenosis aórtica severa sintomática en los 3 laboratorios de cateterismo cardiaco pertenecientes al Centro de Estudios en Cardiología Intervencionista desde marzo de 2009 hasta diciembre de 2020 inclusive (n=122). Se utilizaron los criterios de DUKE modificados para adjudicar la ocurrencia de EI protésica, clasificándose además de acuerdo al tiempo del diagnóstico de la EI en temprana (dentro de los primeros 60 días), intermedia (60 días a un año) y tardía, luego del año. Se evaluaron los datos basales, clínicos y de seguimiento así como el microorganismo hallado. Se utilizó el paquete SPSS v. 17.1 para el análisis estadístico al evaluar los diferentes tiempos de aparición de la EI protésica. La edad promedio de los ptes fue de 82,5 +/- 7,3 años, siendo 52,7% hombres. De las 122 TAVI implantadas, 54,9% fueron autoexpandibles, 83,7% fueron por acceso femoral, el 5,4% tenían implantado un marcapaso previo al procedimiento o requirieron marcapaso definitivo en un 18,4% de los casos. El tiempo de internación fue de 6,4 +/- 5,8 días. El seguimiento de los pacientes luego del alta hospitalaria fue de 1064 +/- 488 días. A largo plazo, la incidencia global de EI protésica fue del 2,4% y el microorganismo hallado en fue el estafilococo epidermidis en dos casos y enterococo faecalis en 1. Se realizó reemplazo valvular convencional exitosamente en un caso, y tratamiento antibiótico en el 100%, con una mortalidad global de la EI del 33%.
Conclusión. La incidencia de EI protésica en nuestra población es baja, similar a los reportes presentados en otros países. La estrategia de profilaxis y tratamiento deben dirigirse a gérmenes habituales para endocarditis.
Keywords: endocarditis infecciosa de válvula protésica, TAVR, TAVI, endocarditis infecciosa.
Los autores declaran no poseer conflictos de intereses.
Fuente de información Colegio Argentino de Cardioangiólogos Intervencionistas. Para solicitudes de reimpresión a Revista Argentina de CardioangiologÃa intervencionista hacer click aquí.
Recibido 2021-06-15 | Aceptado 2021-07-20 | Publicado

Esta obra está bajo una Licencia Creative Commons Atribución-NoComercial-SinDerivar 4.0 Internacional.

Introduction
Currently, the indications for transcatheter aortic valve implantation (TAVI) have gone from the management of inoperable or high-surgical risk patients with symptomatic, severe aortic stenosis to the management of younger low-surgical risk patients with fewer comorbidities with similar results compared surgical aortic valve replacement (SAVR) (1-2). Infective endocarditis (IE) is a rare disease that impacts patients significantly and has high short- and long-term morbidity and mortality rates (3). Patients treated with surgical aortic valve replacement have a higher risk of developing endocarditis. As a matter of fact, almost 20% of all cases of IE occur in patients with SAVR (4). When infective endocarditis takes over prosthetic valves it is considered a severe short- and long-term complication associated with high morbidity and mortality rates that go from 0.3% to 1.2% per year, and a 10-year cumulative risk of 5%. It is more common in bioprostheses compared to mechanical valves (5-9). The information available on the long-term incidence rate of PVIE in patients treated with TAVI is scarce in our region, and the international data on this regard do not included patients from our setting (10-13). The Registry of Infective Endocarditis in Argentina (EIRA 3) published back in 2018 is the largest series of IE ever reported in Latin America. Based on the EIRA, 18.3% of all endocarditis were found in prosthetic aortic valves. However, it did not specify whether the devices studied came from surgical or transcatheter procedures (14).
The objective of this consecutive registry of patients treated with TAVI is to know the long-term in-hospital incidence rate of PVIE, its microbiological profile, and the clinical results in an attempt to assess strategies that may prevent and treat this disease in our region.
Material and methods
Study Design
This is a longitudinal, retrospective, and follow-up registry that evaluated all patients treated with TAVI from March 2009 through December 2020 from 3 Argentine centers. Data were collected from the Centro de Estudios en Cardiología Intervencionista prospective TAVI registry from a web-based database that included a standard case report form with the demographic, clinical, angiographic, and echocardiographic data of all consecutive patients treated with transcatheter aortic valve implantation (Figure 1).
Definitions
The Modified Duke criteria were used to define infective endocarditis, also at the follow-up. The cases reported were assessed together with the internal medicine and infectious disease units to study each case. IE was classified as possible or definitive based on the time elapsed until the event occurred (late, within the first 60 days; intermediate, from day 61 to 1 year; and late, after 1 year).
Endpoints
The study primary endpoint was the incidence rate of prosthetic valve infective endocarditis. The study secondary endpoints included all-cause mortality and stroke after the diagnosis of endocarditis. The microorganisms found and the antibiotic prophylaxis administered were reported too.
fromStatistical analysis
Regarding the statistical analysis, discrete variables were expressed as frequencies (percentage of patients). Continuous variables were expressed as mean and standard deviation. P values were estimated using the Student t test, the chi-square test or Fisher’s exact test, when necessary. The statistical software package SPSS v.17.7 (IBM Corp, Armonk, NY, United States) was used.
Results
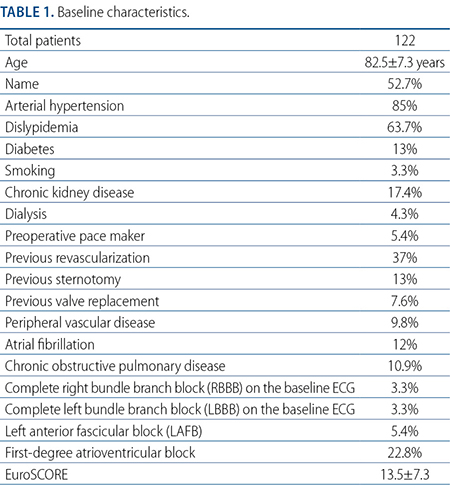
A total of 122 patients treated with TAVI were studied. The median follow-up was 1064 +/- 488 days. The mean age was 82.5 +/- 7.3 years, and 52.7% of the study patients were males. The EuroSCORE was 13.5+/- 7.3. Femoral access was used in 83.7% of the cases being 54.9% of the valves used self-expandable valves. The remaining baseline clinical characteristics are shown on Table 1. This table also includes the baseline electrocardiographic data of the study population. A total of 5.4% of these patients were already carriers of a definitive pacemaker prior to the procedure while 18.4% were implanted with a pacemaker after TAVI; none of these 2 groups had infective complications associated with the device during the procedure or in the long-term. Table 2 shows the procedural characteristics of transcatheter aortic valve implantation. Table 3 shows the long-term overall results. The mean hospitalization time were 6.4 +/- 5.8 days.
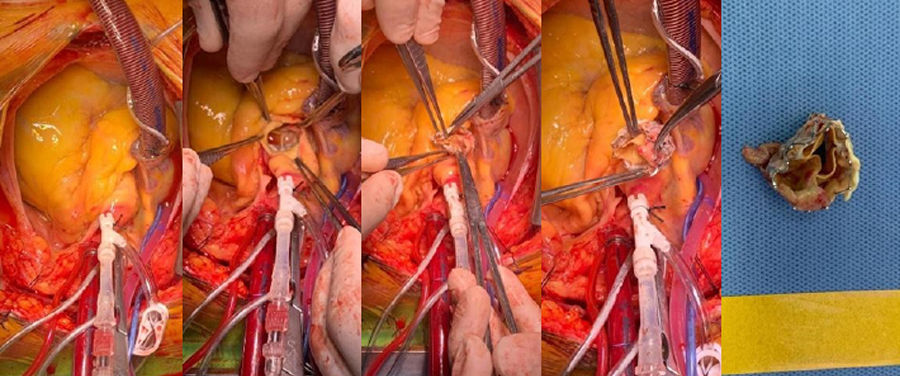
One patient had an early episode of PVIE (within the first 60 days after the procedure), and 2 patients experienced late episodes of PVIE (1 patient after 13 months and the other one 19 months later). The overall rate of PVIE was 2.4%. In all the cases, diagnosis was achieved after confirmation of positive hemocultures and the presence of the lesion in the prosthetic valve as seen on the ECG (1 Jena valve, JENA, Germany, 1 Portico self-expandable valve, Abbott- Saint Jude, United States, and 1 Edwards Sapiens balloon-expandable valve, Edwards-Lifesciences valve, United States). The microorganisms isolated were Staphylococcus epidermidis in 2 cases and enterococcus faecalis in 1. Conventional surgical aortic valve replacement was successful in 1 case (Figure 2) while antibiotics were administered in 100% of the patients with an overall mortality rate for PVIE of 33% due to the occurrence of a stroke during the PVIE-related hospitalization. Figure 2 shows images of valve replacement in the patient with PVIE. Antibiotics were administered to the patient who received conservative management (daptomycin and linezolid). No direct correlation was found between previous surgical procedures and the appearance of endocarditis in any of the 3 patients.
Discussion
The rate of PVIE was studied from the longitudinal registry of consecutive patients from 3 TAVI-capable centers in Argentina and the following findings were reported: first, the 3-year cumulative incidence ratio of PVIE in high-surgical risk patients was 2.4%, which is somehow similar to the rate reported by most results from the registries and reviews published to this date (15). Although the numbers may vary, they never exceed 5% at the 5-year follow-up, which is similar to the rate reported regarding SAVR (3). Back in 2015, a multicenter study published on Circulation reported incidence rates of 0.3% to 1.2% per patient/year while the 2633-patient cohort registry conducted by Butt et al. reported an incidence rate of PVIE of 4.4% at the median follow-up of 3.6 years. On the other hand, the Swedish national registry reported a higher rate of PVIE within the first year of 2.3%, indicative that the higher risk was reported within the first year after implantation. Nonetheless, we did not see these results in our study (10, 15, 16).
Secondly, the microorganisms found were the same ones reported in the series of surgical prosthetic valves (3). In the EIRA-3 registry, the Staphylococcus species were the most common germ followed by Streptococcus and Enterococcus (14). In our registry similar results were reported and the most common germs were Streptococcus (66%) and Enterococcus (33%). In the Swedish series the results reported were similar to those obtained in our registry (18).
Although the implantation of cardiac devices is associated with higher morbidity and mortality rates, as well as with more infections, in our registry, none of the 3 patients were pacemaker carriers (17). Similarly, no direct correlation was seen between previous surgical procedures and the development of PVIE in either one of the patients.
Our registry has some limitations. First, although it is a consecutive series of patients treated by the same group of operators from 3 different centers, the size of the sample is rather small. Secondly, although the registry was prospective in nature, it was conducted to know the procedural characteristics and the long-term results of transcatheter aortic valve implantation without specifically looking for endocarditis. That is why the retrospective search for this entity can be associated with both selection and survival biases.
Unanswered questions on transcatheter aortic valve implantation in the assessment of PVIE still remain since this procedure is not exactly the same as conventional surgical aortic valve replacement. TAVI is a hybrid procedure performed at cath labs that happen to be different from conventional operating rooms regarding asepsis. Also, the preparation, hospitalization, and follow-up of the patients is “stent-like” and, therefore, similar to angioplasty; also, care is similar regarding the previous preparation of the patient and follow-up care. At the beginning of the registry, the use of antibiotic prophylaxis was not regulated as in traditional valve replacement surgeries vs other procedures like dental or diagnostic interventions. Another limitation when it comes to drawing definitive conclusions is that patients treated with TAVI had severe comorbidities that were seen in the risk score used (EuroSCORE). This added to the frailty of this group of patients, which also elevates the risk of infections. We should remember that, in this consecutive series, almost 20% of the patients were treated via transapical access (19), an access site that has fallen into disuse and that is associated with worse short-term results. The only death reported due to early PVIE was a patient in whom this strategy had to be used due to the impossibility of using femoral accesses and an absolute contraindication to surgical aortic valve replacement. Finally, we should not forget that TAVI does not remove the native valve and that, given the special characteristics of this procedure, a macroscopic and microscopic lesion of native endothelium occurs that is adjacent to the valve predisposed to this entity.
Conclusion
In our population, the rate of prosthetic valve infective endocarditis associated with TAVI is low, and similar to the rates already reported in other countries. The prophylactic strategy and treatment used should target the common germs responsible for endocarditis.
-
Mack MJ, Leon MB, Thourani VH, et al. PARTNER 3 Investigators. Transcatheter aortic-valve replacement with a balloon-expandable valve in low risk patients. N Engl J Med 2019;380:1695-705.
-
Popma JJ, Deeb GM, Yakubov SJ, et al. Evolut Low Risk Trial Investigators. Transcatheter aortic-valve replacement with a self-expanding valve in low-risk patients. N Engl J Med 2019;380:1706-15.
-
Murdoch DR, Corey GR, Hoen B, et al. Clinical presentation, etiology, and outcome of infective endocarditis in the 21st century: the International Collaboration on Endocarditis-Prospective Cohort Study. Arch Intern Med 2009;169:463-73.
-
Ostergaard L, Valeur N, Ihlemann N, et al. Incidence of infective endocarditis among patients considered at high risk. Eur Heart J 2018;39: 623-9.
-
Habib G, Thuny F, Avierinos JF. Prosthetic valve endocarditis: current approach and therapeutic options. Prog Cardiovasc Dis 2008;50:274-81.
-
Glaser N, Jackson V, Holzmann MJ, Franco-Cereceda A, Sartipy U. Prosthetic valve endocarditis after surgical aortic valve replacement. Circulation 2017;136:329-31.
-
Ostergaard L, Valeur N, Ihlemann N, et al. Incidence of infective endocarditis among patients considered at high risk. Eur Heart J 2018;39:623-9.
-
Mahesh B, Angelini G, Caputo M, Jin XY, Bryan A. Prosthetic valve endocarditis. Ann Thorac Surg 2005;80:1151-8.
-
Edlin P, Westling K, Sartipy U. Long-term survival after operations for native and prosthetic valve endocarditis. Ann Thorac Surg 2013;95:1551-6.
-
Butt JH, Ihlemann N, De Backer O, et al. Long-Term Risk of Infective Endocarditis After Transcatheter Aortic Valve Replacement. J Am Coll Cardiol 2019;73:1646-55.
-
Olsen NT, De Backer O, Thyregod HG, et al. Prosthetic valve endocarditis after transcatheter aortic valve implantation. Circ Cardiovasc Interv 2015;8:e001939.
-
Amat-Santos IJ, Messika-Zeitoun D, Eltchaninoff H, et al. Infective endocarditis after transcatheter aortic valve implantation: results from a large multicenter registry. Circulation 2015; 131:1566-74.
-
Regueiro A, Linke A, Latib A, et al. Association between transcatheter aortic valve replacement and subsequent infective endocarditis and inhospital death. JAMA 2016;316:1083-92.
-
Avellana PM, García AM, Swieszkowski S, et al. Endocarditis infecciosa en la República Argentina. Resultados del estudio EIRA 3. Revista Argentina de Cardiología, vol. 86, núm. 1, pp. 20-28, 2018.
-
Khan A, Aslam A, Satti KN, Ashiq S. Infective endocarditis post-transcatheter aortic valve implantation (TAVI), microbiological profile and clinical outcomes: A systematic review. PLoS ONE 15(1): e0225077.
-
Amat-Santos IJ, Messika-Zeitoun D, Eltchaninoff H, et al. Infective endocarditis following transcatheter aortic valve implantation: results from a large multicenter registry. Circulation 2015;131:1566-74.
-
Glaser N, Persson M, Dalén M, et al. Long-term Outcomes Associated With Permanent Pacemaker Implantation After Surgical Aortic Valve Replacement. JAMA Netw Open 2021;4(7):e2116564.
-
Bjursten H, Rasmussen M, Nozohoor S, et al. Infective endocarditis after transcatheter aortic valve implantation: a nationwide study. Eur Heart J 2019;40:3263-9.
-
Mieres J, Menéndez M, Fernández-Pereira C, Rubio M, Rodríguez AE. Transapical Implantation of a 2nd-Generation JenaValve Device in Patient with Extremely High Surgical Risk. Case Rep Cardiol 2015;2015:458
A MatÃas RodrÃguez-Granillo
Servicio de CardiologÃa Intervencionista, Sanatorio Otamendi, CABA. Servicio de CardiologÃa Intervencionista, Sanatorio Las Lomas, San Isidro, Provincia de Buenos Aires. Servicio de CardiologÃa Intervencionista, ClÃnica IMA, Adrogué, Provincia de Buenos Aires. Centro de Estudios en CardiologÃa Intervencionista, CABA, Argentina..
Camila Correa-Sadouet
Servicio de CardiologÃa, Sanatorio Otamendi, Ciudad de Buenos Aires, Argentina.
Hernán Pavlovsky
Servicio de CardiologÃa Intervencionista, ClÃnica IMA, Adrogué, Provincia de Buenos Aires. Centro de Estudios en CardiologÃa Intervencionista, CABA, Argentina.
Juan D Orellana
Servicio de CardiologÃa Intervencionista, ClÃnica IMA, Adrogué, Provincia de Buenos Aires, Argentina. 4. Centro de Estudios en CardiologÃa Intervencionista, Ciudad de Buenos Aires, Argentina.
LucÃa Fontana
Servicio de CardiologÃa Intervencionista, ClÃnica IMA, Adrogué, Provincia de Buenos Aires, Argentina. 4. Centro de Estudios en CardiologÃa Intervencionista, Ciudad de Buenos Aires, Argentina.
Carlos Fernández- Pereira
Servicio de CardiologÃa Intervencionista, ClÃnica IMA, Adrogué, Provincia de Buenos Aires. Centro de Estudios en CardiologÃa Intervencionista, CABA, Argentina.
Juan Mieres
Servicio de CardiologÃa Intervencionista, Sanatorio Las Lomas, San Isidro, Provincia de Buenos Aires. Centro de Estudios en CardiologÃa Intervencionista, Ciudad de Buenos Aires, Argentina.
Norberto G Allende
Servicio de CardiologÃa, ClÃnica IMA, Adrogué, Provincia de Buenos Aires, Argentina.
Valeria Curotto
Servicio de CardiologÃa Intervencionista, ClÃnica IMA, Adrogué, Provincia de Buenos Aires, Argentina. 4. Centro de Estudios en CardiologÃa Intervencionista, Ciudad de Buenos Aires, Argentina.
Alfredo E RodrÃguez
Servicio de CardiologÃa Intervencionista, Sanatorio Otamendi, CABA. Servicio de CardiologÃa Intervencionista, Sanatorio Las Lomas, San Isidro, Provincia de Buenos Aires.. Centro de Estudios en CardiologÃa Intervencionista, CABA, Argentina..
Autor correspondencia
A MatÃas RodrÃguez-Granillo
Servicio de CardiologÃa Intervencionista, Sanatorio Otamendi, CABA. Servicio de CardiologÃa Intervencionista, Sanatorio Las Lomas, San Isidro, Provincia de Buenos Aires. Servicio de CardiologÃa Intervencionista, ClÃnica IMA, Adrogué, Provincia de Buenos Aires. Centro de Estudios en CardiologÃa Intervencionista, CABA, Argentina..
Correo electrónico: mrodriguezgranillo@gmail.com
Para descargar el PDF del artículo
Incidence rate of long-term infective endocarditis after transcatheter aortic valve implantation
![]() Haga click aquí
Haga click aquí
Para descargar el PDF de la revista completa
Revista Argentina de CardioangiologÃa intervencionista, Volumen Año 2021 3
Revista Argentina de CardioangiologÃa intervencionista
Issue # 3 | Volumen
11 | Año 2021
Welcome to SOLACI/CACI 2021 Scienti...
Alfredo E RodrÃguez
Welcome to XXVI Congress of the Lat...
AnÃbal Damonte
Welcome to SOLACI/CACI 2021 Congres...
Diego Grinfeld
Colchicine and residual inflammator...
Pablo Corral y cols.
Incidence rate of long-term infecti...
A MatÃas RodrÃguez-Granillo y cols.
Valve-in-valve transcatheter aortic...
José MarÃa Milanesi y cols.
Articulos exclusivos web
Abstracts for SOLACI/CACI 2020/2021...
Several authors
Etiquetas
prosthetic valve endocarditis, TAVR, TAVI, infective endocarditis
Tags
endocarditis infecciosa de válvula protésica, TAVR, TAVI, endocarditis infecciosa
Incidence rate of long-term infective endocarditis after transcatheter aortic valve implantation
Autores
A MatÃas RodrÃguez-Granillo, Camila Correa-Sadouet, Hernán Pavlovsky, Juan D Orellana, LucÃa Fontana, Carlos Fernández- Pereira, Juan Mieres, Norberto G Allende, Valeria Curotto, Alfredo E RodrÃguez
Publicación
Revista Argentina de CardioangiologÃa intervencionista
Editor
Colegio Argentino de Cardioangiólogos Intervencionistas
Fecha de publicación
2021-09-30
Registro de propiedad intelectual
© Colegio Argentino de Cardioangiólogos Intervencionistas